YOUR JAW, HEAD AND NECK PAIN COULD BE TMD
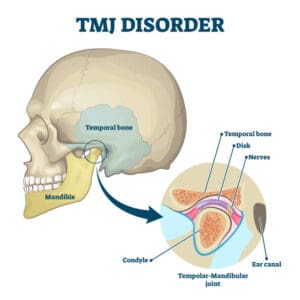
The temporomandibular joint is the joint that connects your jaw to your skull. When this joint is injured from a blow to the jaw or strained due to poor habits like bruxism/clenching of the jaw, even poor postural habits, it can lead to pain, and this is called temporomandibular joint (TMJ) syndrome. It is also known as myofascial pain dysfunction or temporomandibular joint disorder (TMD)
Causes of temporomandibular joint (TMJ) syndrome:
Injury to the teeth or jaw, misalignment of the teeth or jaw, teeth grinding/bruxism, poor posture, stress, arthritis, and gum chewing to name a few
Signs and symptoms of temporomandibular joint (TMJ) syndrome may include:
- Pain or tenderness in the jaw, especially at the area of the joint with chewing
- Jaw clicking and popping and crepitus
- Nerve irritation resulting in facial pain
- Ear pain/earache/fullness in the ears
- Popping sounds in ears/cracking/ringing called tinnitus
- Headaches or blurred vision
- Stiff or sore jaw muscles
- Pain in the temple area
- Locking of the jaw joint, dislocation or subluxation of the TMJ
- Pain that feels like a toothache
- Tight, stiff, or sore neck muscles
- Facial pain, mouth pain, jaw pain, cheek pain, or chin numbness or tingling
- Pain at the base of the tongue
- Difficulty chewing
- Shoulder pain
- Locking or dislocation of the jaw (usually after widely yawning), referred to as lockjaw
- Dizziness or vertigo
The prognosis for TMJ syndrome is generally good as the disorder can usually be managed with conservative treatment, self-care and home exercises. A physiotherapist with a special interest in this disorder can assist with assessing and guiding your management of the condition.
What are the risk factors for TMJ syndrome?
- Poor posture in the neck and upper back muscles may lead to neck strain and abnormalities of jaw muscle function as these areas are related biomechanically.
- Stress may increase muscle tension and jaw clenching.
- Women 18-44 years of age have increased risk.
- Patients with other chronic inflammatory arthritis have increased risk.
- People with jaw trauma like a blow to the jaw
- People who have a genetic predisposition to pain sensitivity and increased stress responses may be more susceptible.
- Prolonged time in an opened position of the jaw like when having dental work done.
- Misalignment (malocclusion) of or trauma to the teeth or jaw,
- Teeth grinding (bruxism),
- Orthodontic braces
- Gum chewing.
How do health-care professionals diagnose TMJ syndrome?
A physiotherapist with a special interest in TMJ dysfunction can diagnose TMJ syndrome by taking a detailed medical history and doing a physical exam to find the cause of the symptoms. A referral to an oral and maxillofacial specialist, or a dentist specializing in jaw disorders may be recommended by your physiotherapist if additional assessment or investigations are required. Sometimes an MRI of the temporomandibular joint may be ordered to detect damage to the cartilage of the jaw joint and to rule out other medical problems.
A condition that may have some similar symptoms to TMJ syndrome is trigeminal neuralgia. The trigeminal nerve supplies nerve impulses to the temporomandibular joint, and when irritated, it can also cause facial pain. Other causes of face or neck pain include swollen lymph nodes (swollen glands), arthritis, salivary gland disease, sore throat or ill-fitting dentures to name a few.
A wholistic approach is needed in treating TMJ dysfunction.
Treatment for TMJ Syndrome:
TMD oftens responds well to Conservative treatment. A physiotherapist trained in this area can assist with rehabilitation of this disorder and some advice/treatment may include:
- Jaw exercises to strengthen muscles of the jaw and/or neck
- Exercises to improve flexibility, and range of motion of the jaw and/or neck
- Roccobado exercises for the TMJ
- Specific manual joint mobilisation techniques performed by your physiotherapist trained in these techniques. These are aimed at reducing pain, improving range and nutrition to the joint. Also important in the case of disc derangement
- Stress reduction
- Heat therapy
- Trigger point therapy and soft tissue mobilisation techniques for the muscles including intraoral techniques.
- Dry needling for trigger points. This is especially helpful for the hard-to-reach muscles of the jaw and requires highly skilled needling techniques.
- Advice including diet modifications and other self-help techniques
- Dental splint (occlusal splint or stabilization splint or bite guard), which is a dental appliance placed in the mouth that keeps the teeth in alignment and prevents tooth grinding. This splint is usually fitted by a maxillofacial surgeon or dentist with a special interest in this area.
- Cognitive Behavioural Therapy [CBT] may help diminish pain intensity.
- In severe cases, surgery on the jaw or dental surgery may be necessary. This is the last resort and seldom performed.
- TMJ arthroscopy or arthrocentesis is a minimally invasive procedure usually done in an outpatient setting.
- Prescription-strength medicines may be used to treat TMD
What is the prognosis for TMJ syndrome?
The prognosis for TMJ syndrome is good. There are numerous causes for TMJ syndrome, so the outlook depends on the cause, if known. Often it can be well managed with a little physiotherapy, self-care and some simple modifications.
In severe situations, where pain is chronic, or associated with other inflammatory disorders, long-term treatment may be necessary to manage the condition and an interdisciplinary approach is required.
Your physio at Scarborough:
Nicolette Visser has a special interest in the TMJ and headaches and has been treating these disorders for over 15 years. She has done numerous courses related to the topic (including Dr Steven Stavrou’s comprehensive TMJ course) and collaborated closely with maxillofacial surgeons and dentists to achieve good outcomes for her patients. She is also a highly skilled Dry Needling practitioner and if required, uses this intervention as part of her management of TMD.
Book a consultation with Nicci Visser online at this link or call us on 0738801649 to book.
After being a patient of Nick Schuster’s and Mel’s for many years and receiving amazing care, I am so excited to know that Nicolette has a special interest in TMJ Disorder! With my TMJ disorder recently becoming substantially worse, I am looking forward to meeting Nicolette next week!
Thanks so much Scarborough Physio and Health!